Introduction
Follicular lymphoma (FL) has a highly variable clinical course. Chemoimmunotherapy can induce durable remissions, but ~20% relapse early. The PI3K pathway is central to FL biology and multiple PI3K inhibitors (PI3Ki) are approved for FL, but the molecular profile of tumors most sensitive to PI3Ki is unknown. Further, PI3Ki are dosed indefinitely which contributes to toxicity and cost. Copanlisib is an IV inhibitor of PI3Kα and δ isoforms with high activity in relapsed FL. We hypothesized that patients with FL tumors most sensitive to PI3Ki will achieve deep and durable remissions after a fixed duration of copanlisib-based therapy. Here we report preliminary results of a response-adapted study using copanlisib and rituximab as frontline therapy for FL.
Methods
Pts with untreated grade 1-2, 3A FL, ≥stage 2, and any tumor burden are eligible if they meet criteria for need of systemic therapy that includes symptoms, increasing size of nodes, critical organ involvement, or impending organ compromise. No prior systemic therapy other than radiation is permitted. Frozen or archival tissue is required. Eligibility includes age ≥18 and adequate organ function unless involved by FL. Active HIV, CMV, Hep B or C, and autoimmune conditions requiring therapy are excluded. All pts receive PCP prophylaxis. Pts first receive copanlisib 60mg on days 1, 8, and 15 of a 28-day window to test activity of monotherapy. On-treatment tumor biopsies are optional after the window. Following the window, pts receive 6 cycles of copanlisib 60mg on days 1, 8, and 15 of a 28 day cycle along with rituximab 375mg weekly x 4 then on day 1 of each cycle. Streck tubes for circulating tumor DNA (ctDNA) are collected weekly during the window, after each cycle, and during surveillance. FDG-PET and CT scans are performed at baseline, after the window, and after cycles 3 and 6 to determine response. Patients with complete response (CR) after 6 cycles stop therapy. Patients with partial response (PR) after 6 cycles receive another 6 cycles of combination therapy with the copanlisib reduced to day 1 and 15 of each cycle. Non-responding patients will receive standard chemotherapy. The primary endpoint is the overall rate of CR with secondary endpoints of safety and duration of CR. Exploratory objectives include identification of a signature that predicts PI3Ki response.
Results
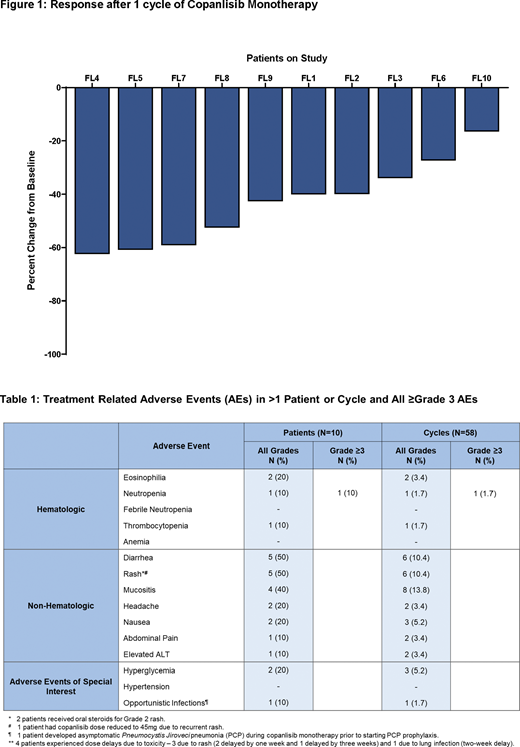
Ten pts have been enrolled and completed the copanlisib window. Median age was 50y (range, 28-77) including 3 (30%) over age 70. Seven (70%) pts had high-risk FLIPI scores ≥3 and two (20%) pts had Grade 3A FL. Comorbid conditions included prediabetes in 4 (40%) and hypertension in 4 (40%). All 10 (100%) pts had tumor reductions during copanlisib monotherapy with a median reduction of 41% (range 16-62%) (Figure 1). Four pts have completed 6 cycles of copanlisib and rituximab and all 4 (100%) have responded including 2 (50%) who achieved CR. In the two pts who achieved a PR after 6 cycles, one had a 90% tumor reduction and one had only persistent minimal residual disease in the bone marrow by flow cytometry. Toxicity was evaluated in 10 pts across 58 cycles and the most common have included rash (50%), diarrhea (50%) and mucositis (40%) which have all been G1 or G2 and successfully managed with supportive care and did not recur with subsequent cycles. One pt developed grade 3 neutropenia that responded to growth factors and did not recur. Four pts had dose delays due to rash (N=3) and lung infection (N=1). One pt had copanlisib reduced to 45mg due to recurrent rash and elevated liver tests. No pt has discontinued therapy. One pt required oral diabetic medications during therapy that were stopped after therapy completed. One pt had asymptomatic PCP pneumonia diagnosed during the copanlisib window prior to starting prophylaxis that was successfully treated while therapy continued.
Conclusion
Copanlisib is highly active in untreated FL and the first 10 (100%) patients all had tumor reductions after the first cycle of copanlisib monotherapy, including patients with high tumor bulk. Combination of copanlisib and rituximab can induce complete responses after only 6 cycles and without indefinite therapy. The safety profile includes rash and diarrhea that respond to supportive care and lessen on subsequent cycles. Updated clinical results from this ongoing trial (NCT03789240) along with the molecular profile of FL tumors will be presented at the meeting.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal